Newborn Jaundice: A Condition Overview
Detecting and Treating Newborn Jaundice: A Guide for Medical Equipment Buyers
Globally over 100,000 late-preterm and term babies die each year because of jaundice, a condition caused by hyperbilirubinemia, which is elevated bilirubin in the bloodstream (1). About 60% of full-term newborn and 80% of premature babies have jaundice, and in many cases especially among term babies, jaundice resolves without intervention in a couple days if there are no other underlying health conditions. However, there are greater risks for small or premature babies.
By understanding the diagnosis and management of jaundice, and products that can help support these important interventions, medical distributors can expand access to high-quality healthcare for newborns and their families, and prevent long-term complications and disabilities from jaundice.
Globally over 100,000 late-preterm and term babies die each year because of jaundice.
What Medical Product Buyers Need to Know About Newborn Jaundice
Jaundice happens when a chemical called bilirubin (yellow pigment of red blood cells) builds up in the baby’s blood. During pregnancy, the mother’s liver removes bilirubin for the baby, but after birth the baby’s liver must remove the bilirubin, in some babies the liver might not be developed enough to get rid of bilirubin. When too much bilirubin builds up in a new baby’s body, the skin and whites of the eyes might look yellow. This yellow coloring is called jaundice.
Most infants develop visible jaundice due to elevation of unconjugated bilirubin concentration, or “hyperbilirubinemia” during their first week. This is called physiological jaundice and is the most common type as it can happen with no additional or underlying health conditions.
- Term infants: jaundice lasts for about 10 days with a rapid rise of serum bilirubin up to 204 μmol/l (12 mg/dL).
- Preterm infants: jaundice lasts for about two weeks, with a rapid rise of serum bilirubin up to 255 μmol/l (15 mg/dL).
Key Terms: Infant Jaundice
Bilirubin
When the liver breaks down old red blood cells bilirubin is produced in the body.
Hyperbilirubinemia
An abnormally high level of bilirubin in the blood demonstrated by jaundice and lethargy.
Jaundice
Kernicterus
A severe health condition that occurs with excessively high bilirubin levels which can move into the brain tissue and cause permanent damage and injury.
All infants at risk, or suspected of having elevated bilirubinemia, should have a laboratory test of serum bilirubin to diagnose jaundice and guide treatment with phototherapy. However, in many resource-constrained settings that is not feasible, so alternative methods, such as bilirubinometers (jaundice meters) or other point of care methods are more practical for both diagnosis of jaundice and for monitoring phototherapy treatment.
The Importance of Diagnosing Jaundice
Early identification of infants at risk of severe hyperbilirubinemia is an essential component of newborn care; all newborns should be examined within 24 hours of birth and in the following two days. Parents and healthcare workers should be encouraged to look for jaundice by blanching the skin (on the nose in particular), looking at the gums and examining the eyes.
Risk Factors Depend On:
Gestational age of baby at time of birth
Other health conditions (e.g. asphyxia temperature instability, sepsis)
Visual inspection of the skin or eyes (sclera) is an instant and cost-free way of estimating the serum bilirubin, and can be useful for screening but it has limitations in accuracy particularly for screening non-white newborns.
The gold standard to measure hyperbilirubinemia and inform treatment is a laboratory evaluation of serum bilirubin. A blood sample is drawn from the newborn and sent to a lab for testing. Depending on the patient’s proximity to a laboratory facility, this can be both expensive and time-consuming.
Read our Buyer’s Guide on Newborn Jaundice Diagnostics to find out more about jaundice diagnostics and the top considerations to make when selecting the right product for your clinical setting.
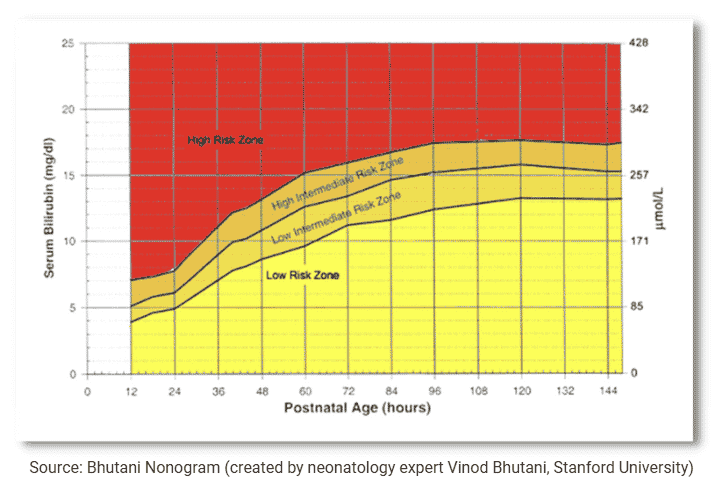
Newborn Jaundice Risk Zones
Products for Diagnosing Jaundice
Bilirubinometers are point-of-care devices that can be used to diagnose jaundice quickly wherever the patient is. The most common type of bilirubinometer is transcutaneous (also known as a jaundice meter). These devices offer a non-invasive, and inexpensive way to estimate total serum bilirubin. Their measurement of higher bilirubin concentrations is limited and they are therefore recommended only as a screening tool for full-term infants (9).

Recently, minimally invasive point-of-care (POC) bilirubinometers have been developed that enable healthcare providers to both accurately diagnose jaundice and guide treatment in settings where laboratory testing is not a realistic option. Testing a few drops of whole blood delivers results within minutes. Moreover, these devices can test serum bilirubin before and during phototherapy treatment.

Recently, minimally invasive point-of-care (POC) bilirubinometers have been developed that enable healthcare providers to both accurately diagnose jaundice and guide treatment in settings where laboratory testing is not a realistic option. Testing a few drops of whole blood delivers results within minutes. Moreover, these devices can test serum bilirubin before and during phototherapy treatment.
Treating Newborn Jaundice with Phototherapy: Effective and Early Treatment Can Save Lives and Prevent Long-Term Health Consequences
Although many newborns will have jaundice (hyperbilirubinemia) which may resolve without intervention, if severe jaundice is left untreated, it can cause neurologic damage and a condition called kernicterus. Phototherapy (and in more extreme cases exchange transfusion) is well-established as the most effective treatment for severe newborn jaundice (hyperbilirubinemia) (7).
Diagnosing jaundice is an important newborn intervention, however without access to phototherapy, facilities and providers are limited in their ability to treat severe jaundice. Equipping facilities that treat infants with adequate phototherapy machines is essential for comprehensive newborn care.
Severe jaundice and kernicterus are preventable with prompt treatment, but it is estimated that at least 114,000 infants die every year from hyperbilirubinemia, and more than 63,000 live with permanent neurological impairment. Most of these are concentrated in lower-resource countries (8).
Phototherapy uses blue light wavelengths to treat unconjugated hyperbilirubinemia and is necessary to prevent morbidity and mortality from dangerous levels of neonatal jaundice. Bilirubin absorbs the blue light and is then broken down in the blood, allowing the infant to excrete the excess bilirubin before it can accumulate and cause permanent irreversible health issues.

VIA Global Health is committed to supporting health systems access affordable and appropriate medical products to improve the health in their communities. Products included in our Buyers Guides are available for purchase at VIA Global Health
References and Acknowledgments
(1) Olusanya, BO; Teeple, S; Kassebaum, NJ (February 2018). “The Contribution of Neonatal Jaundice to Global Child Mortality: Findings From the GBD 2016 Study”. Pediatrics. 141 (2): e20171471. doi:10.1542/peds.2017-1471. PMID 29305393.
(2) National Institutes for Health and Clinical Excellence. Neonatal jaundice. (clinical guidelines 98), 2010.
(6) National Collaborating Centre for Women’s and Children’s Health. Neonatal Jaundice: NICE; 2010.
(9) Dowsett, Laura E. et al. “Transcutaneous Bilirubinometers for Newborn Hyperbilirubinemia: A Health Technology Assessment”. University of Calgary. 2017 Jan 30
