Buyers Guide
Devices for Supplemental Oxygen Accessories for Regulation and Conditioning (Flowmeters, Flow-splitting devices, Humidifiers)
Importance of Oxygen Accessories for Oxygen Regulation and Conditioning
As part of comprehensive systems for oxygen therapy, flowmeters, flow-splitting devices and humidifiers are important in regulating and conditioning oxygen before it is delivered to the patients, and are covered in this Buyers Guide. These accessories that control flow and humidity are particularly important when using an oxygen concentrator or oxygen with newborns; managing low flow is critical to longer term health issues.
Selection, utilization, and integration of these devices will depend on a number of factors, such as oxygen source, clinical use, and the resources at the health facility. Much more detail about these devices is available through this document WHO-UNICEF Technical Specifications and Guidance for Oxygen Therapy Devices (2019), a resource which VIA recommends for distributors and end-users of oxygen therapy.
Special consideration must be given when extra oxygen or “supplemental oxygen therapy” is needed for infants born with respiratory distress. While oxygen supplementation can be life-saving, it can also be toxic and have long-lasting effects, especially with newborns or low birthweight babies. Extreme care should be exercised when administering oxygen to any patient, particularly newborn infants, even for a short amount of time to ensure low enough flow and appropriate concentration.
UNICEF has developed an Excel-based tool for healthcare facilities and procurement officials to plan for their oxygen needs, from source to delivery and understand what solutions might be available to increase their oxygen availability.
Types of Oxygen Accessories
Flowmeters
Flowmeters are devices that measure and control the rate of oxygen flow to a patient, and may be used with piped oxygen, cylinders, or oxygen concentrators, though typically oxygen concentrators have integrated flowmeters. There are three types of oxygen flowmeters: Thorpe tube; Bourdon gauge; and dial/click, all of which come with varying flow ranges. For newborns, and particularly premature babies, ultra-low flow ranges should be 0-200 mL/Minute (or 0-1 L/minute) and with graduations of 20 mL/min. Higher flow ranges and graduations are more appropriate for low-flow applications and newborn or pediatrics, (0-5 L/minute) and 0-15 L/min for higher flow applications.
Thorpe tubes are the most commonly used flowmeters, also known as rotameters. They connect to a gas source, and have a valve to control gas flow rate, an upright tube with a float to measure gas flow, and an outlet port. The figure below represents different configurations based on oxygen source and use case.
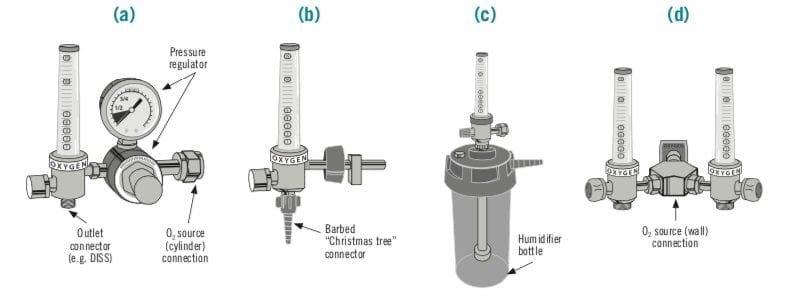
Source: WHO and UNICEF, 2019.
Considerations for Purchasing Flowmeters
- Other accessories. In addition to the flowmeter itself, a pressure-reducing valve, outlet adapter, and humidifier, depending on the use case, may also be required
- Compensated vs uncompensated flowmeters. Compensated flowmeters have the advantage of indicating when the system is delivering insufficient oxygen, for example if the line becomes obstructed or there is a kinked tube, and is therefore a safety measure for oxygen therapy. Uncompensated flowmeters would erroneously show a high flow rate due to increased gas under the float
Flow Splitters
Flow-splitting devices enable oxygen from a concentrator or another source to be split among multiple patients, while still monitoring and adjusting individual flow rates. It is important to make sure that each “output” has the same Fi02 (inspired oxygen) as the gas source to which it is attached. For neonates, low flow (0-2 L/min) oxygen administration is important for health and safety of the newborns. Splitters and flowmeters should also have adjustment at minimum of 0.1-0.125 L/min.
Types of Flow Splitters
- Flowmeter stand: Also known as a flowmeter station or assembly, distributes medical oxygen, from a single source to multiple outlets through independent flowmeters, which can be adapted to individual patient needs, each outlet should have precise controls and visual indications for monitoring. These devices are useful for concentrators or where there are limited oxygen sources
- Dual Flowmeters distribute medical oxygen by splitting output flow from a piped oxygen, or terminal unit, oxygen source through two independently regulated flowmeters, to meet

Source: WHO and UNICEF, 2019.
Oxygen Humidifiers
Oxygen humidifiers are medical devices can be incorporated into oxygen delivery systems to humidify supplemental oxygen, particularly for higher flow rates or when oxygen delivery bypasses the nose, as is the case when nasopharyngeal catheters are used. Humidification is typically not necessary when oxygen is delivered at relatively low flow rates through nasal prongs or nasal catheters. How oxygen humidifiers fit into the more broad system is important, especially to ensure safety and mitigate risks.
Considerations for purchasing oxygen humidifiers
There are various types of oxygen humidifiers, which differ based on three main principles related to humidification: temperature; surface area; and time of contact.
Types of oxygen humidifiers
- Reusable non-heated bubble humidifiers: these are simple, low-cost devices that add water to oxygen gas by bubbling the gas through water at room temperature, allowing pressurized oxygen gas to flow down a tube into the bottom of a water container. From there, the gas escapes from the distal end of the tube forming bubbles that gain water vapor as they rise to the surface. These must be filled with clean water (distilled water or tap water that has been boiled and cooled), and then firmly attached to the oxygen outlet and are important to use with higher flow oxygen or use of a nasopharyngeal catheter
- Single use non-heated bubble humidifier functions in a similar manner as the reusable except the bottles are not reusable. This may reduce bacterial contamination.

- Heated humidifiers, because they have a heat source and a humidification chamber can warm the water in the chamber to add moisture to the airstream as it passes over the water surface. Both CPAP and high-flow nasal cannula (HFNC) oxygen therapy require heated humidification and a blender, though some devices have built in humidification.
- Managing Infection Risks. Very careful infection prevention precautions must be taken to clean, sterilize the chamber and tubing as infections for vulnerable patients can potentially outweigh the benefits of this technology.

VIA Global Health is committed to supporting health systems access affordable and appropriate medical products to improve the health in their communities. Products included in our Buyers Guides are available for purchase at VIA Global Health.
References and Acknowledgments
(2) WHO-UNICEF Technical Specifications and Guidance for Oxygen Therapy Devices (2019)
